| ✅ Reviewed by Dr. Tom McCawley | 🕒 Reading time: three minutes |
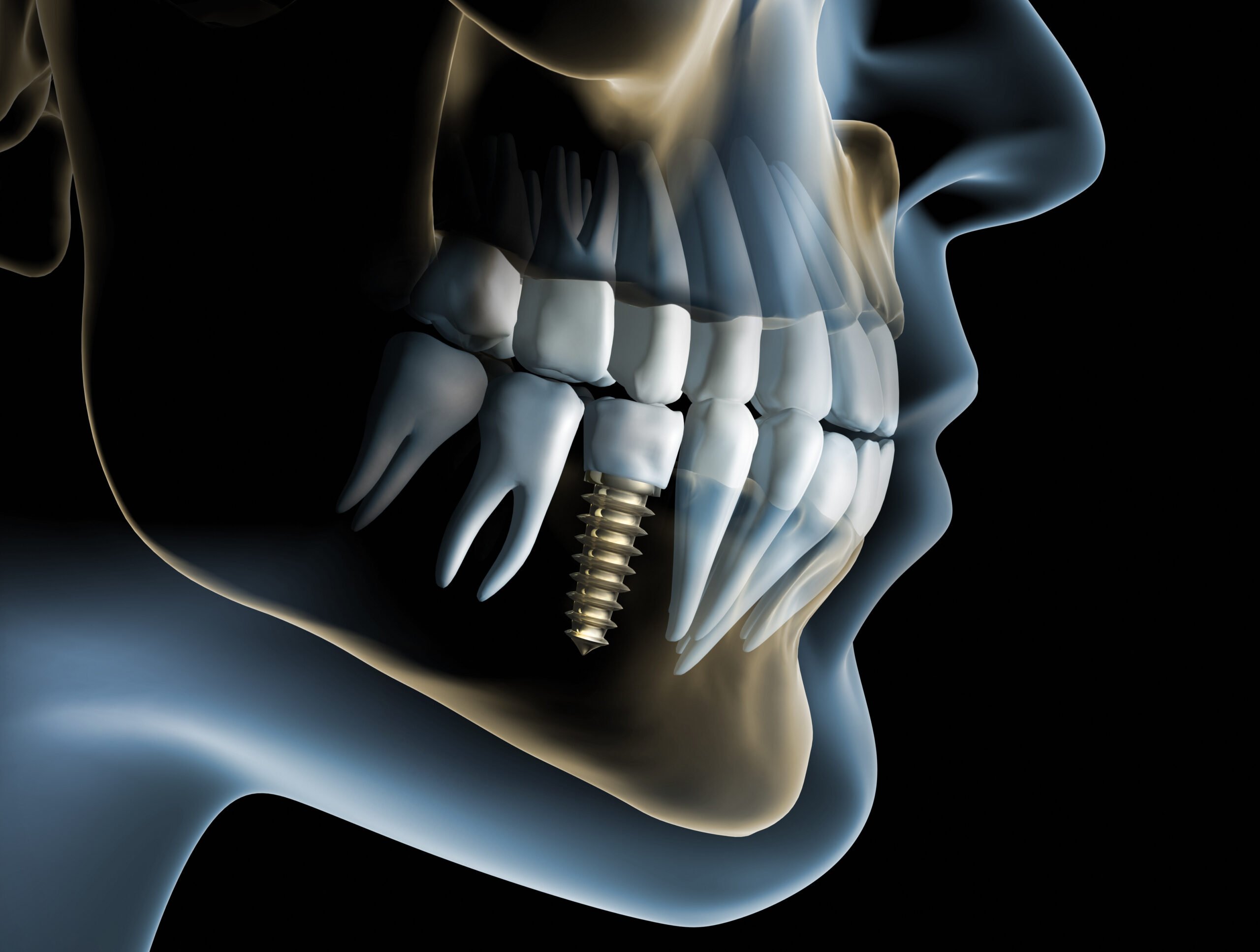
Dental implants are built to last for decades, but their long-term success depends on the health of your gums and jawbone. Even though implants aren’t natural teeth, they can still face similar challenges, especially when harmful bacteria build up around them.
Gum Disease vs. Peri-Implantitis: What’s the Difference?
Both gum disease and peri-implantitis are bacterial infections that damage the tissues supporting your teeth or implants. The main difference is what they affect.
Gum disease (periodontitis) develops around natural teeth when bacteria build up under the gumline and begin destroying the surrounding bone and connective tissue. Peri-implantitis is gum disease that occurs around dental implants when bacteria collect near the implant post, leading to inflammation and bone loss.
While both conditions cause bleeding, swelling, and deep pockets around the gums, implants are more at risk once bone loss begins. Unlike natural teeth, they do not have a ligament that helps protect and anchor them in place.
Early Warning Signs of Implant Infection
Because implants don’t have nerves like natural teeth, symptoms can be subtle. Watch for:
- Bleeding when brushing or flossing
- Red or swollen gums around the implant
- Tenderness or pain when chewing
- Receding gums exposing the implant threads
- Persistent bad breath or unpleasant taste
If these symptoms sound familiar, you may be experiencing peri-implant mucositis, the reversible early stage of infection before bone loss occurs.
What Causes Peri-Implantitis?
Peri-implantitis develops when bacteria or inflammation damage the tissue around an implant. Common contributing factors include:
- Inadequate cleaning around the implant, which allows bacteria to build up.
- Previous gum disease, which increases the risk of infection returning.
- Smoking or vaping, which limits blood flow and slows healing.
- Health conditions such as diabetes or immune disorders that affect the body’s ability to fight infection.
- Bite problems or poorly fitted restorations that place stress on the implant or trap bacteria.
Even patients with excellent oral hygiene can develop peri-implantitis if there is a bacterial imbalance or hidden infection deep below the gumline.
How We Treat Peri-Implantitis
Early diagnosis is key. At our Fort Lauderdale periodontal office, we use advanced tools to target infection before it compromises your implant:
- Microscopic bacterial analysis to identify harmful bacteria
- Laser therapy (LAPIP®) to remove infected tissue without surgery
- Targeted antimicrobial therapy to eliminate bacteria at the source
- Supportive maintenance programs every 3–6 months to protect implant health
These treatments not only stop infection but also help preserve surrounding bone and tissue, reducing the risk of implant loss.
| Our approach to implant care is unique because we specialize in treating the complex conditions that often surround implant cases, such as gum disease, bone loss, and peri-implantitis. Rather than focusing solely on the placement of implants, we prioritize infection control, long-term stability, and preserving oral health whenever possible. |
How to Prevent Implant Infections
Healthy habits are the best protection against future implant problems.
- Brush and floss daily, using an interdental brush and water flosser to clean around the implant.
- Schedule professional cleanings and exams at least twice a year.
- Do not smoke or vape. If you do, make a plan to quit—tobacco use greatly increases the risk of implant failure.
- Keep systemic conditions such as diabetes under control.
- Report any bleeding, swelling, or gum changes as soon as you notice them.
Implant infections can develop slowly, even years after placement. Staying proactive with your care helps prevent long-term complications and keeps your implants strong and stable.
Schedule a Periodontal Exam in Fort Lauderdale, FL
While dental implants don’t develop periodontal disease in the traditional sense, they can develop peri-implantitis, a bacterial infection that behaves similarly. The good news? With early diagnosis and specialized care, peri-implantitis is treatable and often reversible.
To book an appointment at our periodontal office in Fort Lauderdale, FL, call (954) 807-4829 or visit us at 800 East Broward Blvd #706 Fort Lauderdale, FL.
FAQs
Watch for bleeding, swelling, or soreness around the implant. Persistent bad breath or a bad taste may also signal infection. Any redness or inflammation of the soft tissue around the crown should be checked immediately.
Because implants lack nerves, you might not feel pain until bone loss becomes advanced. However, if you notice gum recession or changes to the gum contour near the implant, it could be a sign of ongoing inflammation.
Early-stage inflammation (peri-implant mucositis) can often be reversed with professional treatment and improved home care. In more advanced cases, regenerative procedures such as bone grafting or laser therapy may be used to rebuild lost support and improve implant success.
Peri-implantitis should be treated by a periodontist who specializes in implant infections. At the McCawley Center for Laser Periodontics & Implants, we use the LAPIP® laser protocol to target bacteria, preserve bone, and help save implants that might otherwise be lost.